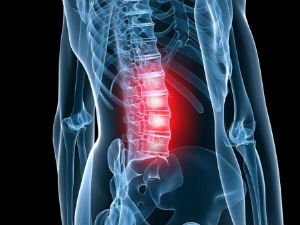
According to medical statistics, lower back pain in 80% of cases is caused by lumbar osteochondrosis. This occurs as a result of degenerative-dystrophic changes in this segment, when the intervertebral discs and the adjacent vertebrae are affected. Osteochondrosis of the lumbar spine (OBOP) manifests itself in a variety of symptoms: pain of a different nature, limitation of mobility, impaired sensitivity of the lower body, etc. With prolonged absence of treatment, degenerative processes spread to the vertebrae, reducing the ability to work, then the patient may become disabled.
To avoid dangerous complications of lumbar osteochondrosis (LP), you need to start complex treatment at 1-2 stages of pathology. In advanced cases, when irreversible changes in the disc or vertebrae are already present, an operation is performed. To avoid osteochondrosis of the lower back, and the associated complications, it is necessary to carry out its prevention.
Development of lumbar osteochondrosis
To understand what is osteochondrosis of the Lumbar Spine (Lumbar Spine), you need to study the structure of the spinal column. It consists of vertebrae, between which are placed cartilaginous pads (intervertebral disc). The disc is covered with a hard fibrous membrane (annulus fibrosus), inside which is the nucleus pulposus. This structure has a shock-absorbing function and makes the spine more flexible.
Help. The lumbar segment of the spine is subjected to tremendous stress on a daily basis, as it supports the weight of the upper body. Therefore, osteochondrosis of the lower spine is diagnosed more often than the cervical, thoracic.
With regular stress on the spine, the discs contract, lose a lot of fluid, their height decreases, and the distance between the vertebrae decreases. The cartilaginous lining becomes fragile, microcracks appear on its surface, through which the nucleus pulposus protrudes over time. With further compression of the intervertebral discs, the outer shell ruptures and the gelatinous body falls out, so a hernia is formed. Then there is pathological mobility of the vertebrae, the load on the adjacent segments of the spine increases.
A little later, bone growths (osteophytes) begin to form at the edges of the vertebral bodies. Thus, the body tries to stabilize the spine.
Doctors distinguish 4 stages of osteochondrosis of the lumbar spine:
- 1 degree - problems with discs begin, the central part dehydrates, it flattens, cracks appear on the outer shell. Has an erased current.
- 2 degree - the cartilaginous lining sags, the vertebrae come closer to each other, become more mobile, the muscles and ligaments around the spine sag. Pain appears.
- 3 degree - protrusions, hernias, and subluxations of the vertebrae are formed. The pain increases, mobility is limited, the sensitivity of the lower body is disturbed.
- Degree 4 osteochondrosis is characterized by the appearance of osteophytes that can damage the spinal nerves and adjacent vertebrae. There is constant pain, severe neurological disorders and other complications, the risk of disability increases.
The easiest way to cure chondrosis of the lower back (stage 1), however, it is very difficult to identify the disease at this stage. Intervertebral osteochondrosis of the 2nd degree is treated using conservative techniques. Surgery may be required at stages 3-4.
Help. According to statistics, OBO is more often detected in patients after 30 years. There are frequent cases of the development of pathology in people after 20 years. Approximately 80% of patients 60 years old suffer from manifestations of this disease.
Reasons
To understand how to deal with osteochondrosis PKOP (lumbosacral spine), you need to know its causes:
- Regular static or dynamic load on the lumbar segment. The risk group for the development of osteochondrosis includes office workers, professional athletes (weightlifting), movers, builders, etc.
- Poor posture, prolonged inappropriate posture.
- Genetic predisposition, abnormalities in the formation of the vertebral bodies. This category includes youthful software - curvature of the spinal column caused by pathologies of the vertebral bodies.
- Spinal column injuries.
- Hormonal imbalance, metabolic disorders, diseases of the endocrine glands, which disrupt metabolism in the lumbar segment.
- Age-related changes in the body provoke disc wear.
- Bone tuberculosis, osteomyelitis (purulent inflammation of the bone tissue), ankylosing spondylitis (inflammation of the vertebrae and joints), rheumatoid arthritis, etc.
A disease is often caused by several causes.
In addition, there are factors that provoke the development of lumbar osteochondrosis:
- Overweight.
- Passive lifestyle, prolonged sitting.
- Regular use of unhealthy foods (fatty, fried foods, confectionery, semi-finished products, etc. ).
- Lack of fluid, dehydration.
- Congenital disorders of the structure of the spine, for example, an additional vertebra.
- Regularly wearing uncomfortable heels.
- The period of gestation, then the load on the spinal column increases.
- Abrupt refusal to train professional athletes or excessive sports in people who previously led a passive lifestyle.
- Smoking, frequent and excessive drinking.
There are many more factors that can trigger degenerative-dystrophic processes in the lumbar spine. For example, flat feet, frequent hypothermia of the back, frequent stress, sleep disorders, etc.

Symptoms
Symptoms of osteochondrosis of the lumbar spine are diverse, they depend on the stage of pathology and localization of the affected area.
Physicians distinguish reflex and compression syndromes (complex of symptoms) in OBOR. The former arise when the receptors of the outer shell of discs, ligaments, joint capsules are irritated, and the latter, when the nerve bundles, blood vessels, and spinal cord are compressed.
There are such reflex syndromes of lumbar osteochondrosis:
- Lumbago. Shooting pain in the lower back with sudden movement or exertion. At the slightest attempt to move, the pain syndrome intensifies, so the patient freezes in one position. The muscles in the damaged area are very tense, with palpation, the painful sensations become more pronounced. These manifestations are associated with the movement of the nucleus pulposus inside the outer shell.
- Lumbodynia. The aching pain develops for several hours or days. Discomfort increases with movement, change in body position. It is weakened when a person takes a horizontal posture with a roller under the lower back. When raising a straight leg in this position, the pain increases (Lassegh's symptom). The degree of muscle tension is less than with lumbago. The mobility of the lower back is limited.
- Lumboischialgia. Painful sensations (sharp or aching) spread from the lower back to the lower body. There is an increase in this sign during movements. The pain is relieved by resting on the back. The muscles in the affected area are tense, the pain syndrome becomes pronounced on palpation.
Symptoms of compression syndromes depend on which parts of the lumbar segment are damaged. The characteristic signs are associated with compression of the spinal nerves by hernias, osteophytes, displaced vertebrae. This condition is called radiculopathy, in which the pain increases with the slightest movement, the muscles of the lower back are strained, and mobility is limited.
Clinical manifestations of compression syndromes depending on the damaged vertebrae of the lumbar segment:
- L1 - L3 - pain and numbness in the lumbar region, front and inner thighs, the patient has difficulty bending / unbending the leg at the knee.
- L4 - pain syndrome extends to the front of the thigh, descends to the knee (behind). In the same area, sensitivity is disturbed.
- L5 - painful sensations radiate to the buttocks, the outer part of the thigh, descend along the front of the lower leg to the inner part of the foot and the big toe. In the same area, numbness is felt, it is difficult for the patient to bend the big toe.
- S1 - pain spreads from the lower back to the buttock, the outer and back of the thigh, descends to the outer part of the lower leg, foot. In the same areas, numbness is felt, the muscles of the lower leg are weakened, so it is difficult for the patient to stand on his toes.
There is a risk of damage to several nerve bundles at once, for example, L5, S1. If the hernia moves backward, it can compress the spinal cord.
Compression of blood vessels in the lower back increases the likelihood of weakening of the leg muscles, numbness of the lower extremities, impaired control over the process of urination and defecation. In men with OBO, erection is impaired, and in women, the main symptoms may be supplemented by inflammation of the ovaries or uterus.
Diagnostic measures
To diagnose OBOP, the doctor examines the patient, palpates the patient to determine the condition of the muscles and to identify the curvature of the spine. It is important to tell the specialist in detail about your symptoms to make it easier for him to diagnose.
Instrumental examinations will help to detect intervertebral osteochondrosis:
- X-ray of the lower back (frontal and lateral projection).
- Computed and magnetic resonance imaging.
X-ray allows you to assess the structure of the EPP. To detect abnormal mobility of the vertebrae, x-rays are taken in flexion and extension positions. This study allows us to notice that the intervertebral fissure has narrowed, the vertebral bodies have shifted, and osteophytes have appeared on their edges. However, this diagnostic method is considered obsolete.
Today, CT and MRI are increasingly used to detect degenerative-dystrophic changes in the spine. These highly informative studies make it possible to assess the condition of the vertebrae, discs, intervertebral foramen, and the spinal cord. With their help, protrusions, the direction of the hernia, the degree of compression of the nerve bundles, spinal cord, and blood vessels are detected.
Treatment
MEDICINES FOR LUMBAR OSTEOCHONDROSIS

Treatment of osteochondrosis EPP lasts from 1-3 months to 1 year. The success of therapy depends on the patient himself, who must strictly follow the doctor's recommendations. With self-medication, the patient's condition usually worsens.
Treatment goals:
- Stop or mitigate software symptoms.
- Identify the cause of the disease, try to exclude it from life.
- Eliminate the inflammatory process.
- Restore blood circulation, metabolic processes in the lumbar spine.
- Try to improve the condition of damaged cartilaginous lining, stop further degenerative changes.
To achieve such goals, it is recommended to carry out a complex therapy. It usually starts with taking medications:
- Muscle relaxants. They relax muscles, relieve pain and inflammation.
- NSAIDs. They have anti-inflammatory, analgesic, antipyretic effects.
- Antispasmodics. They help to stop smooth muscle spasm, relieve pain.
- Anesthetics. They are used for severe pain syndrome in the form of a therapeutic blockade.
- Glucocorticosteroids. They also help to cope with pain. However, these drugs are capable of destroying bones, so they are taken for a short time and only after a doctor's approval.
- Sedatives. They relieve neuromuscular tension, improve sleep.
- Vitamins (group B, E, C, A). Restores the condition of the affected nerves, relieves pain.
Careful. NSAIDs are prohibited from taking with gastritis or stomach ulcers, as they further damage the mucous membranes of the gastrointestinal tract.
In case of an exacerbation, the patient is given injections, and after the relief of the main symptoms, he takes oral medications.
In addition, external agents are used (gels, ointments, creams, rubbing).
The question of what to do in case of chronic low back osteochondrosis is quite relevant. If OBOP has become chronic, then after the relief of the main symptoms, the patient is prescribed chondroprotectors, drugs that restore blood circulation, drugs based on vitamins B. They help restore innervation, normalize blood supply to the affected area, and prevent further development of pathology.
Treatment of chondrosis of the lumbar spine (stage 1) is carried out with the use of chondroprotectors, which slow down the development of degenerative processes, accelerate the regeneration of cartilage. In addition, the patient is prescribed vitamin and mineral complexes. This form of osteochondrosis is the easiest to cure.
OTHER CONSERVATIVE TECHNIQUES
In case of acute chronic disease (osteochondrosis) of 1 - 2 degrees, the following treatment procedures will help stop its development:
- Ultrasound therapy relieves pain and inflammation, and normalizes blood flow in the damaged area.
- Detensor therapy is a safe traction of the spine due to the weight of one's own body, after which muscle tone normalizes, and mobility improves.
- Magnetotherapy reduces pain and inflammation of the muscles around the spine.
- Reflexology (insertion of needles into bioactive points on the body) accelerates blood circulation, relieves inflammation and edema.
- Manual therapy (impact on the affected area with the hands of a doctor) and massage normalize muscle tone, reduce compression of nerve bundles, improve the nutrition of intervertebral discs, and restore the structure of the spine.
- Electrophoresis allows the delivery of medicinal solutions through the skin to bone and cartilage tissues.
- Drasonalization improves blood circulation, metabolic processes, reduces pain, restores skin sensitivity.
There are many more effective procedures that will help improve the patient's condition in 5-15 sessions. The main thing is to get a doctor's approval before performing them.
TREATMENT WITH SOFTWARE AT HOME
If you are wondering if it is possible to treat OBO at home, talk to your doctor. If the specialist has given permission, then begin therapy, which usually consists of the following points:
- Diet. If lumbar osteochondrosis is caused by impaired blood flow or metabolism, then exclude fatty, fried, spicy foods, eggs, etc. from the menu. Replenish the menu with fresh vegetables, fruits, lean meat, fish, and dairy products. Give up alcohol, tonic drinks (tea, coffee). Drink filtered water, compotes, herbal teas.
- To restore blood circulation, exercise or apply rubbing and compresses.
- Sleep on an orthopedic mattress, a low pillow. If you have a sedentary job, buy a chair with a back that will support your spine. Wear special corsets or belts from time to time.
- Exercise therapy will help strengthen the muscle corset, relieve some of the load from the diseased spine. The complex for each patient is individually compiled by a doctor or instructor.
- Self-massage the lumbar region. However, ask a professional how to do it right.
- Use folk remedies in the form of rubbing, compresses, baths, etc.
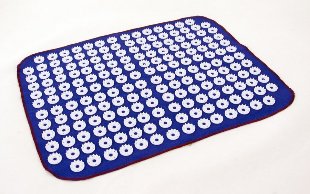
- The needle applicator is a plastic plate with many thorns, which improves blood circulation, metabolic processes in the damaged area, reduces muscle pain, and relaxes.
And also at home you can use lotions with herbal decoctions, plasters.
Help. A novelty in the treatment of osteochondrosis is a massager bed that is suitable even for the most disorganized patients.
However, remember that home treatment can only be done with the permission of your doctor.
SURGICAL TREATMENT
An operation for lumbar osteochondrosis is prescribed if conservative techniques have proven ineffective for a long time. And also surgical intervention is indicated for involuntary urination, defecation and cauda equina syndrome (pinching of the nerves of the lower spinal cord).
The following surgical methods are used in the treatment of OBO:
- Spondylodesis - fusion of adjacent vertebrae.
- Facetextomy - removal of intervertebral joints that pinch the spinal nerve.
- Laminectomy is the removal of the lamina that covers the spinal canal that compresses the spinal cord.
- Discectomy is the complete or partial removal of an intervertebral disc that causes compression of the nerve root or spinal cord.
- Corpectomy - removal of the vertebral body and adjacent cartilage pads. Then the empty space is filled with a bone graft and 3 vertebral segments are fused.
Help. After surgery, there is a risk of complications: spinal cord injuries, nerve bundles, broken grafts, infections, etc.
After treatment, you need to undergo rehabilitation in order to speed up your recovery.
Complications
In the absence of proper therapy, the risk of such complications of lumbar osteochondrosis increases:
- Herniated disc, pinched nerve root or spinal cord.
- Prolonged inflammation increases the likelihood of developing radiculitis (inflammation of the nerve roots).
- Sciatica (inflammation of the sciatic nerve), in which there is severe pain and numbness in the lower limb.
- In case of impaired blood circulation in the spinal cord, the likelihood of compression myelopathy increases (compression of the spinal cord by various formations: bone fragments, hernia, tumors, hematoma).
- Cauda equina syndrome - compression of the roots of the lower spinal cord, which leads to disruption of the functionality of the intestines, pelvic organs, and lower extremities.
To avoid such complications, you need to start treatment as early as possible.
Prevention
To avoid lumbar osteochondrosis, follow these rules:
- Lead a moderately active lifestyle (walk more often, exercise regularly, sign up for a pool).
- For sedentary work, warm up every 1. 5 hours.
- Sleep on an orthopedic mattress.
- Avoid excessive physical exertion, lift weights only from a half-squat position, before that, put on a special belt on your lower back.
- Buy orthopedic shoes.
- Eat right, take vitamin and mineral complexes as prescribed by your doctor.
- Learn to relax.
- Try not to get hypothermic.
- Treat diseases that can cause OBO in time.
- Give up bad habits.
By following these recommendations, you can avoid degenerative changes in the spine and improve your health.
Most Important
If you notice symptoms of lumbar osteochondrosis, see your doctor immediately. Self-treatment can make your condition worse and cause complications. Lumbar chondrosis (stage 1) is treated with exercise therapy, physiotherapy and chondroprotectors. At later stages, drugs, massage, manual therapy, etc. are used. In the absence of positive dynamics for a long time or the appearance of neurological symptoms, the doctor may prescribe an operation. The patient must strictly follow the doctor's recommendations in order to speed up the recovery.




































